As part of the PATIenTS program, the RUISSS Université de Montréal is launching its project to improve the trajectory of people without a family physician using the Guichet d’accès à la première ligne. Dr. Marie-Thérèse Lussier, Clara Dallaire, Viviane Tran, Marie-Hélène Goulet and Dr. Ariane Murray, respectively co-scientific director, patient partner co-director, coordinator, young researcher leader and clinician-intervenor of the SSA-RUISSS Université de Montréal team of the Unité de soutien SSA Québec, will ensure that the project is aligned with the priorities of the Ministry of Health and Social Services and of the Unité and that it fosters partnership and the promotion of the patient perspective.
SSA_RUISSS Université de Montréal team:
- Dr. Marie-Thérèse Lussier
- Clara Dallaire
- Marie-Hélène Goulet
- Viviane Tran
CIUSSS de l’Est de l’Île-de-Montréal :
- Caroline St-Denis
- Anne Dubé
- Marie-Pier Lehoux
Département régional de médecine générale
- Dr. Ariane Murray
- Martine Fournier
Ministère de la Santé et des Services sociaux
- Mélanie Lapointe
- Dominique Perron
- Dr. Réal Barrette
- Rana Farah
Communication expert – Discutons-Santé
- Claude Richard
Guichet d’accès à la Première ligne (GAP)
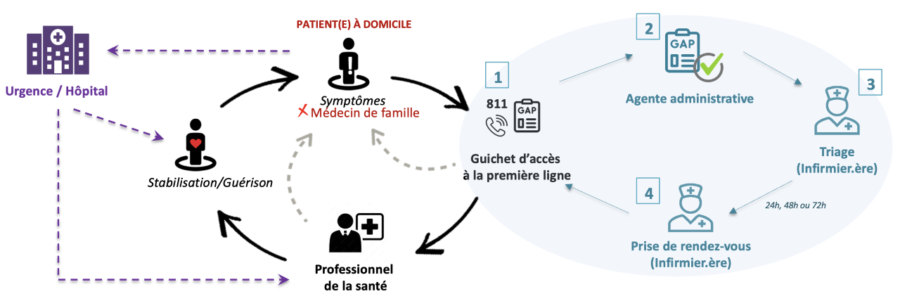
Launched in 2022 by the Ministry of Health and Social Services (MSSS), the Guichet d’accès à la première ligne (GAP) allows people without a family doctor to obtain a medical appointment or health service.

GAP care and service trajectory
Issues
As part of this project, the SSA-RUISSS Université de Montréal team identified the following issues:
- Asking patients to limit their medical consultation to the discussion of a single problem leads to frustration, especially for patients with multiple problems, thus negatively affecting the patient experience
- Encountering orphaned patients who have complex needs and/or require more than one visit to stabilize their condition places great pressure on caregivers
- There are no mechanisms in the GAP to document the post-initial consultation trajectory and follow-ups required for stabilization of the patient’s condition
Objectives
To address these issues, the team aims to achieve two goals:
- Améliorer la communication entre les patientes et les patients et le personnel soignant afin de :
- Making consultations more efficient
- Improve the patient experience
- Reduce pressure on healthcare staff
- Document the necessary actions following an initial medical consultation referred by the GAP
How can we continuously improve the trajectory for people without a family physician using the Primary Care Access Portal?
As part of its PATIenTS project, the SSA-RUISSS Université de Montréal team proposes two concrete improvements:
- Integrate the Medical Appointment Preparation Form (FPRM) (DiscutonsSanté.ca – Capsana) into the GAP trajectory to
- Helping patients
- Actively preparing patients for the consultation offered by GAP helps to improve their experience of care
- It is important to identify the priority issue for discussion
- Supporting the health care staff
- By having access to the FPRM form prior to the consultation, caregivers will be better able to plan the consultation and adjust quickly to the demand
- Promote a patient-professional partnership
- Improve communication at the time of consultation
- Contribute to the efficiency of the meeting
- Helping patients
- Document the trajectory after the initial medical consultation
- To better anticipate the nature and duration of follow-ups required by the patient’s health status, particularly in cases where stabilization of chronic or complex problems is targeted
- Soliciting collaboration with a subset of patients with complex or chronic problems who have been referred by the GAP to:
- Access clinical-administrative data from the electronic medical record (EMR)
- Access the FRPM form (long version) to reflect patient experience (preparation history, notes and comments)
- In order to better anticipate the actual workload of the nursing staff:
- Conclude the episode of care for which the orphan patients were referred to them by the GAP
- Manage the necessary resources

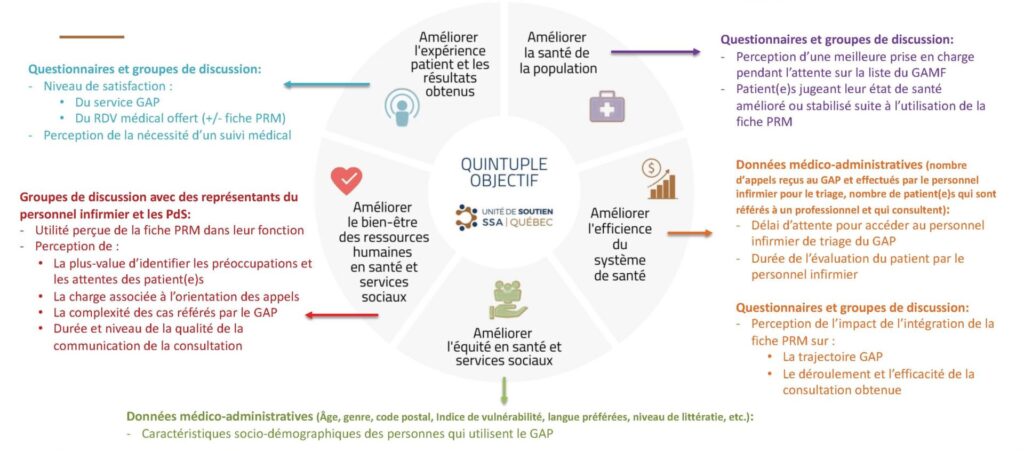
Impact Measurement
As part of the RUISSS PATIenTS project, the project team identified elements that could be measured to assess the impact of the project on each of the elements of the quintuple aim. PDSA continuous improvement cycles (plan, do, check and react) are planned.
PATIenTS Program
The Unité de soutien SSA Québec is launching the Life Trajectory Improvement and Innovation Partnerships in Transition to Sustainable Health (PATIenTS program) in collaboration with the four integrated university health and social services networks (RUISSSs). Through the PATIenTS program, the activation of the Québec learning health system is being carried out in the RUISSS territories of Québec through four tangible projects over a one-year period.
